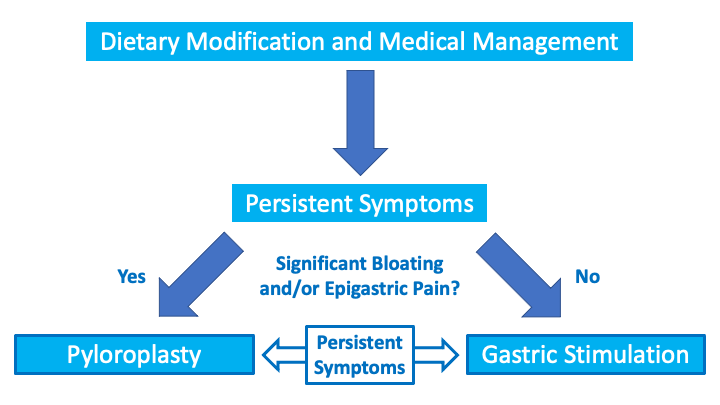
Gastroelectrical Stimulation Procedure
What is it?
After the pyloroplasty procedure, anti-nausea medications often become more effective. For those that cannot control their nausea with medications after pyloroplasty, Dr. Hughes and his team may recommend surgically implanting the Medtronic Enterra II gastric stimulator. The gastric stimulator helps the nerves in the stomach function more normally to empty the stomach more effectively and lessen nausea.
How does it work?
This procedure involves placing two gastric stimulator electrodes in the lower third of the stomach. The electrode leads are then connected to a generator that is placed under the skin in the abdominal wall next to the navel. We also resect a portion of the stomach to count the number of nerve cells to determine why gastroparesis did not respond fully to pyloroplasty and to help determine the best possible settings.
What’s involved?
This is also done laparoscopically as an outpatient procedure. We will start you out on the lowest settings and increase by a small amount every 1-2 months until your nausea is controlled. The settings are adjusted in our clinic by placing a programmer on your skin over the generator. We increase in a slow and gradual manner to find the lowest possible settings that are effective. Since the stimulator is battery powered and not rechargeable, we need to surgically replace the generator whenever the battery becomes depleted. Lower settings result in longer battery life and fewer surgeries to replace the generator.

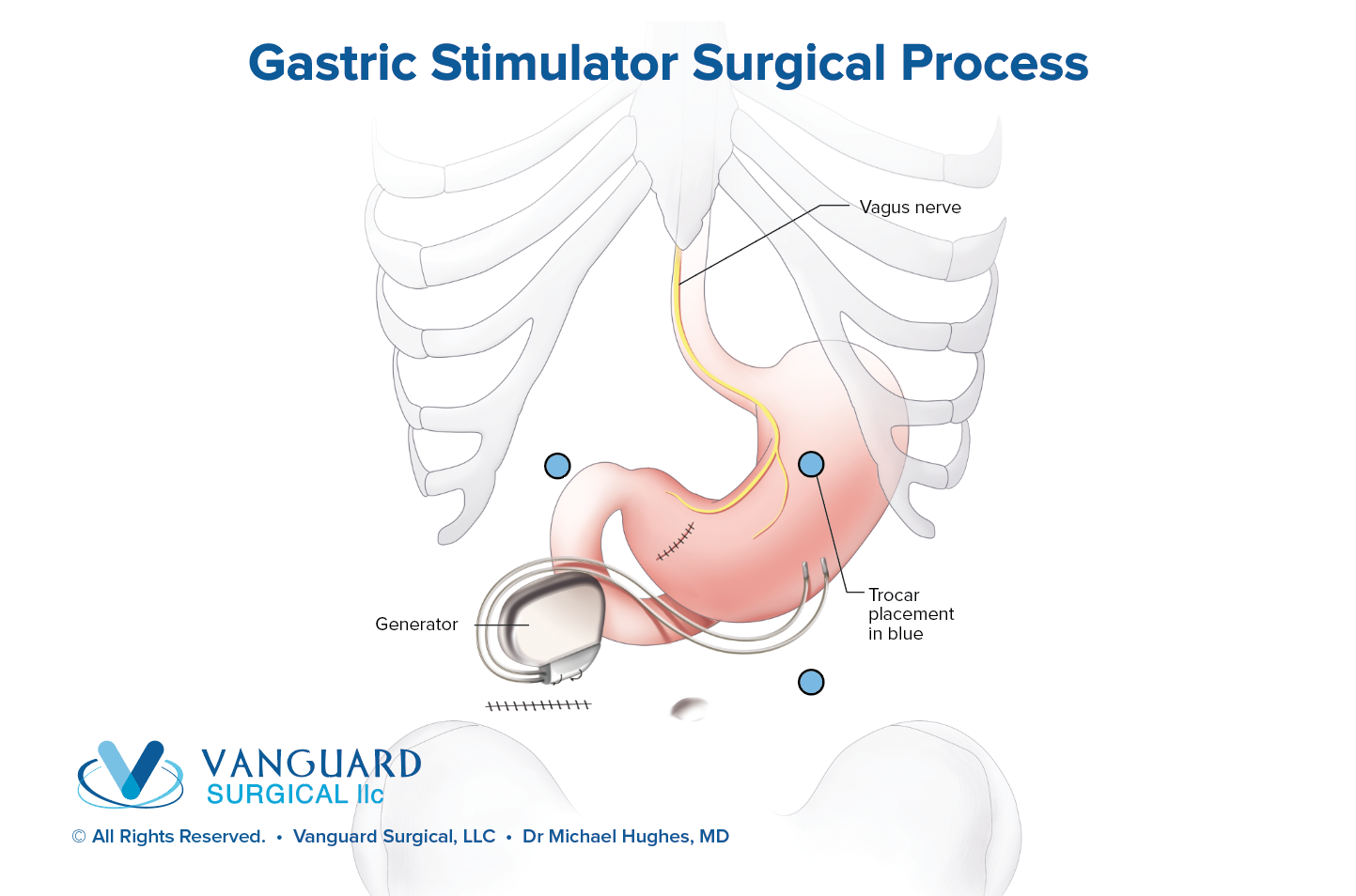
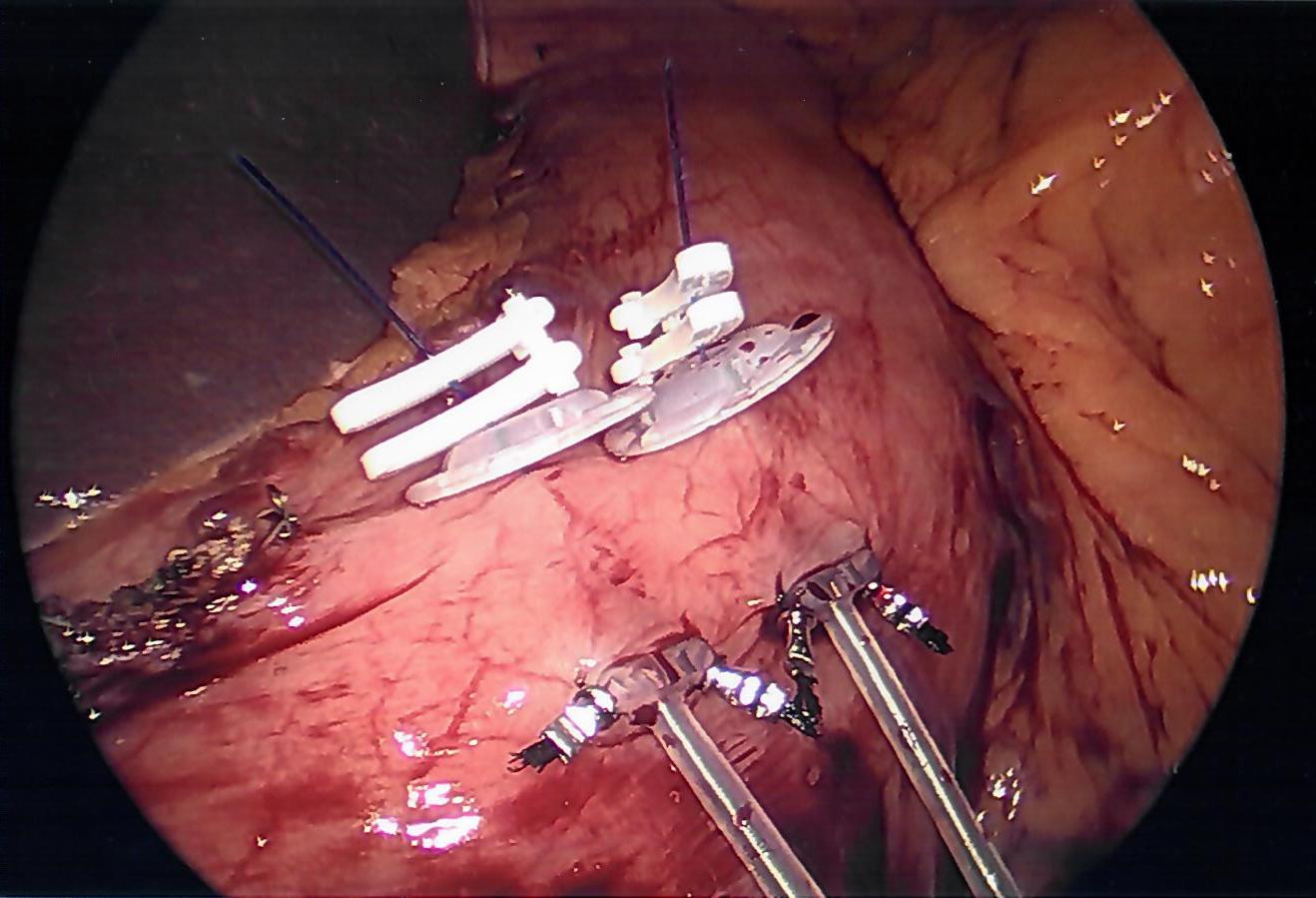
Gastric stimulator leads implanted into stomach wall to restore funtion to the Interstitial Cells of Cajal (stomach pacemaking cells)

Leads covered by fat to prevent them from rubbing into the abdominal wall and from stray electicity shocking the abdominal muscles

What can I expect?
It may take just a few weeks for your nausea to improve on the lowest settings, up to 12 months on the highest settings, or something in-between. When the stimulator is first placed, there may be swelling and fluid that collects around the generator. As it heals, the generator will start to flip or move under the skin. While this is normal and expected, you may find this aggravating.
What are the risks?
The main risk is device infection (10% experience this) that could require removal or reoperation (1%). During stimulator placement, Dr. Hughes will cover the leads with fat to prevent the leads from rubbing. Despite this, you may develop pain on the left from the leads rubbing underneath your ribs or abdominal muscles and may need the system replaced into an alternative location. The device could also need to be replaced if the device fails or if the leads erode all the way into the stomach.
What if gastric stimulation does not help me?
If gastric stimulation does not help you and you have not had a pyloroplasty, then we can perform a pyloroplasty to help the stimulator work better. If you have already had a pyloroplasty, then we need to determine whether there are any medical therapies to help your body respond better to gastric stimulation. With gastric stimulation and/or pyloroplasty, we can get more than 90% of patients at least 50% better.